The small meeting room at Ahoada Primary General Hospital fills quietly as mothers living with HIV settle into their seats, their children leaning against them, many of those children already fighting the same virus. These gatherings, once supported by wider outreach programs, have become a lifeline in a region where funding is thinning and distances are unforgiving.
The counsellor leading the session reminds the women of the rules that keep them alive: take your drugs every day, miss none, protect your babies. Some nod gently. Others stare at their laps. A few tighten their grip around their restless toddlers.
When the session ends, the stories begin unfiltered, weary, and threaded with resilience.
One young mother, who found out she and her newborn were HIV-positive shortly after childbirth, struggles to hold back tears as she switches between Pidgin and pauses that grow heavier with each sentence.
“I cried the day I noticed,” she recalled.
“When I come to collect the drugs, I dey cry. They would tell me make I give her the drugs, and me I should take my own, make I no miss am any day.”
Then she breaks off, describing the financial obstacles weighing her down.
“Now my husband no get work, me too I don’t have anything to do. When they call me sometimes I need to come, but because of transport, I miss. When the drugs finish I don’t take any again, until I get money for transport before I come.”
Another mother says her baby was gravely ill before anyone discovered the source of the sickness. The infection was already advanced only after tests came back did she learn that she too was HIV-positive.
“I didn’t know I was sick too,” she said.
She spoke softly about the harsh reality of rural life.
“Sometimes we cannot come to the health centre to pick up our drugs. I wish the facility would resume sending the medications directly to our homes. That way, we won’t miss our treatment.”
Across Ahoada and Oshigbokor, the pattern repeats: long distances, empty pockets, and shrinking community outreach are forcing families into dangerous lapses in treatment.
The Workers Who Hold the Line
Adherence counsellor and HIV advocate, Amarachi Felix, confirmed what I had already seen.
“From Ahoada down to Oshigbokor is ₦3,000. Going and coming is ₦6,500. I can afford my transport, what about those that don’t have anything?”
She explains how outreach once softened these barriers, until the funding stopped.
“We normally went to communities, but now, no more going.
Most of our patients do not follow up, and some of them are very ill. Each time we went there, we encouraged them, we even paid their transport.
But now, since there is no support, there are a lot of losses and gaps.”
She chairs the Association of Women Living with HIV and explained that only a few community health workers are available to cover the 32 villages in the area.
Inside the support group meeting, I saw how much these gatherings matter. The coordinator, Beatrice Livingstone, told me:
“The support group is where we share experiences and encourage one another.”
She proudly added that women have gained knowledge, confidence, and even jobs through the group.
“For now, we are not seeing positive children among our members because of the health talks,” she said.
Ahoada New Zonal Hospital, Rivers State — July 19, 2025. Photo: Martha Okere
A Story of Hope and Survival
Among the women was 36‑year‑old Innocent Praise, who has lived with HIV for years but whose three daughters are HIV‑negative. She recalled the stigma she faced as a teenager:
“The nurse on duty that day when she found out I was positive was like, ‘small girl like you, you dey waka-waka. Say, how come you go get HIV? You know say HIV dey kill?’
Her mother recognized her symptoms immediately, falling hair, rashes, fatigue and fought beside her.
“As I started taking my drugs and my mother kept supporting me, buying me drugs, my dad, brother, everybody in my family started showing me love.
From there I picked up and I started recovering. When I got pregnant, people even praised me, saying the pregnancy looked good on me. I registered for care and I had access to my drugs.”
Stories like hers are becoming harder to find.
Shrinking Donor Support and Growing Risks
For years, donor funding was the backbone of HIV interventions across Nigeria.
But that support is shrinking fast. Nigeria’s allocation from the Global Fund has dropped by 11 per cent, leaving more than $100 million in unmet needs for HIV, tuberculosis, and malaria programs. And when the U.S. paused foreign assistance in January, access to medicines and prevention services tightened even further.
In Rivers State, the reality of these cuts is already visible.
At an event in Abuja, Dr. Stanley Idakwo, Project Director of the Rivers ASPIRE Project, explained:
“Around 31.7 per cent of women cite distance to facilities as a barrier, 20.1 per cent mention transportation costs, and 16.5 per cent report long waiting times.”
Idakwo explained that those challenges were being mitigated through task-sharing among healthcare workers, improved case management, and integration of PMTCT with broader maternal and child health services across the state.
NEPWAN's Warning from the Field
The Network of People Living with HIV in Nigeria (NEPWAN), Rivers State chapter, says HIV Testing Services is the only community program already feeling the impact of reduced funding.
The state NEPWAN Chairman, Blessing Chigozie, says many Local Government Areas no longer have test kits. She explains that NEPWAN cannot confirm any increase in PMTCT cases, but women in hard-to-reach areas still prefer traditional birth attendants, TBAs who often do not test for HIV.
“One of the biggest challenges is that these people have a challenge. Because if we don't have this drug, how do they sustain their life, how do they live?”
She calls on the state government to provide test kits and open channels of dialogue.
“It's only when people get tested that they can be able to lead to care and get treatment… So we are pleading with the government… They should be able to give us a space with them to sit on the round table to talk and let them hear from these people how they are being fed as regards to their needs and their life and family.”
For NEPWAN, even reaching communities is a struggle.
“NEPWAN as a network does not have mobility, we are restricted… If they can give us a car that can take us to communities, we are not asking for money just that.”
She adds that stigma still drives people away from treatment.
“People are being stigmatized… you see them not coming out to take their drugs… it is affecting the community themselves.”
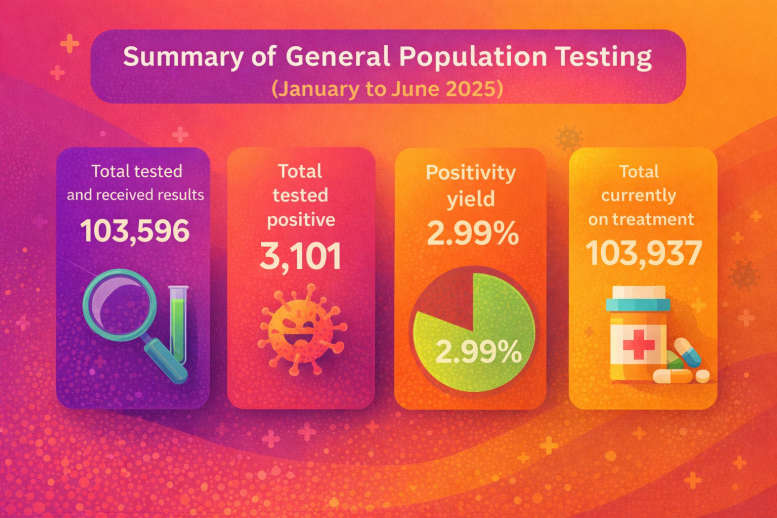
Data Source: State AIDS, Viral Hepatitis and STI Control Program, Rivers State Ministry of Health. Created by Martha Okere with AI assistance
Today, Rivers State has 234,715 people living with HIV.
Health workers are afraid of what these funding cuts mean for mothers like the ones in Ahoada. Even traditional birth attendants are feeling the strain. In Ahoada, a popular TBA known as Nurse Deborah said she has not received HIV test kits for the past two months.
Nurse Deborah said in pidgin English, “Two months ago they said that they get misunderstanding for their working place. I thank God na today wey all of them called me say they are coming back on Wednesday. They come two times in a month. It is getting to two months them never come.”
But, the Program Manager for the State AIDS, Viral Hepatitis and STI Control Program, Dr. Ufuoma Edewor, explained that the ministry has trained and equipped selected TBAs across the 23 LGAs.
She assured that the ministry will continue expanding support, advising TBAs still lacking kits to report to their local government health teams.
Edewor said, “We identified TBS in all the 23 local government areas. Sometime earlier this year we trained 5 man teams in the LGAs to be able to supervise.
We don't have coverage of all the TBAs but we have a significant number of all the TBAs currently in our database that have been trained and supported to test it. So we will continue to provide to more that are willing to come aboard.”
She also said that the state has reached 95% testing coverage for pregnant women registered for antenatal care in PMTCT programs, whether in health facilities or with trained TBAs.
“Antenatal coverage we are still struggling to increase our coverage, but for PMTCT, we have been able to produce testing to over 95% of people that have registered for antenatal care”, she said.
On recent claims of an 86% HIV prevalence rate in Rivers, she warned against spreading misinformation.
“We need to stop spreading fake news… you and I know that is not possible, the prevalence for Rivers State still remains 3.6%, the federal government is preparing to have another survey and until that survey is conducted we cannot say anything about the prevalence.
But just to help the public, our positivity rates this year have hovered between 1.9 to 2.7 but we can’t speak clearly to this until another survey is conducted.”
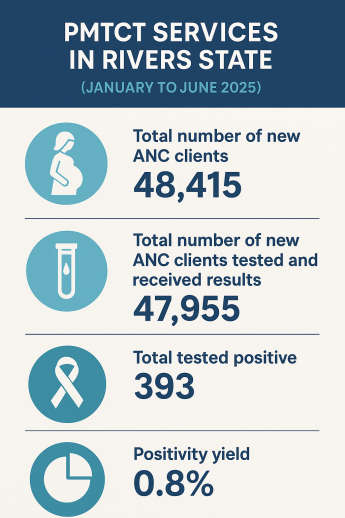
Data Source; State AIDS, Viral Hepatitis And STI Control Program, Rivers State Ministry of Health. Infographics Created by Martha Okere with AI assistance
World AIDS Day - Progress but Also Painful Gaps
In Ahoada, in Oshigbokor, and across rural Rivers State, the story is the same: the fight against HIV is slowly turning into a fight against abandonment. And unless support returns, more mothers and their children will be left behind.
Still, the Rivers State Agency for the Control of AIDS (RIVSACA) says progress has been made.
Project Officer Dr. Naaziga Francis told me that access to treatment today is far better than it was a decade ago.
“We made a whole lot of progress in responding to the HIV situation in River State.
I think all LGAs now have a comprehensive site where people can access one treatment, now they can access what we call the PMTCT service and then people can also be linked to treatment in our 23 LGAs.”
He added that the agency now plans to work with the Greater Women Initiative to strengthen the anti-stigma law.
Also, the Rivers State Ministry of Health says it is stepping up community HIV testing to make sure anyone diagnosed is quickly linked to care and supported throughout their treatment.
The Commissioner for Health, Dr. Adaeze Oreh, says the state has expanded its case-finding efforts across all Local Government Areas to boost early detection and timely treatment.
“Ending AIDs as a public health threat requires every one of us to play a role.
I therefore urge all residents of Rivers State to know your HIV status, support people living with HIV and encourage pregnant women to register early antenatal care and access PMTCT services, challenge stigma, misinformation, and harmful gender norms that hinder progress...”
Dr Oreh went ahead to reel out statistics saying the government is also widening access to HIV services, now available in more than 115 health facilities across the state. She said about 234,715 people are currently living with HIV in Rivers State.
According to her, “Over 81% know their HIV status, 55% of them are receiving life saving anti-retroviral therapy and 98% of those on treatment have achieved viral suppression.
This figure reflects the tremendous work done and the work still required to achieve epidemic control, according to the 2028 national aids indicator and impact survey, our state ranks third in HIV prevalent nationwide with the prevalent rate of 3.6%.”
Meanwhile, data from the State AIDS, Viral Hepatitis And STI Control Program, Rivers State Ministry of Health shows that between January and June 2025, Obio/Akpor LGA led in ANC attendance, with 8,297 new clients, out of which 83 tested positive for HIV and 77 were started on ART.
Port Harcourt City recorded 4,215 new ANC clients, with 45 HIV-positive cases, 43 of whom commenced treatment.
Other LGAs with notable PMTCT interventions include Ikwerre (3,277 ANC clients, 44 HIV-positive, 38 on ART), Akuku Toru (2,233 ANC clients, 9 HIV-positive, 8 on ART), and Ahoada East (2,106 ANC clients, 25 HIV-positive, 22 on ART).
Several LGAs with smaller populations, such as Andoni (434 ANC clients, 4 HIV-positive, 2 on ART) and Tai (1,776 ANC clients, 4 HIV-positive, 2 on ART), also benefited from the HIV testing and treatment programs.
The data shows that the state is making significant strides in Prevention of Mother-To-Child Transmission (PMTCT) services, with 355 HIV-positive pregnant women initiated on antiretroviral therapy (ART) during the period.
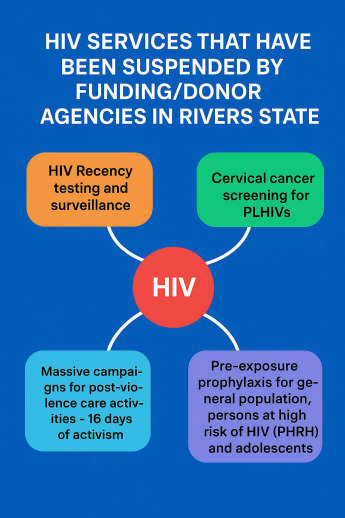
Data Source: State AIDS, Viral Hepatitis and STI Control Program, Rivers State Ministry of Health. Infographics Created by Martha Okere with AI assistance
In 2024, an estimated 40.8 million people were living with HIV globally.
Approximately 630 000 people died from HIV‑related causes in 2024. An estimated 1.3 million people acquired HIV in 2024.
These figures were obtained from the World Health Organization, WHO.
This year’s World AIDS Day theme is: Overcoming Disruption, Transforming the AIDS Response.
According to WHO, after decades of progress, the HIV response stands at a crossroads.
Life-saving services are being disrupted, and many communities face heightened risks and vulnerabilities.
Across Ahoada, Oshigbokor, and rural Rivers communities, mothers are fighting not just HIV, but abandonment.
Their survival depends on a system stretched thin. Until sustainable, government‑led action fills the widening gaps left by donors, the most vulnerable: mothers, babies, and entire communities will remain at risk.
And unless support returns, the cost of inaction may be measured not just in numbers, but in lives quietly slipping away.
Note: This content received support from the Thomson Reuters Foundation as part of its global programme aiming to strengthen free, fair and informed societies. Any financial assistance or support provided to the journalist has no editorial influence.
The content of this article belongs solely to the author and is not endorsed by or associated with the Thomson Reuters Foundation, Thomson Reuters, Reuters, nor any other affiliates.